Bangabandhu Sheikh Mujib Medical University Journal
Volume 16, Issue 4, December 2023
CASE REPORT
Spontaneous
uterine rupture in unscarred uterus in a low resource setting in India: A case
series![]()
Tripura Health Services, Tripura, India
Correspondence to: Dr. Pushpal Chowdhury, Email: dr.pushpalchowdhury@gmail.com
DOI: https://doi.org/10.3329/bsmmuj.v16i4.64534
Received: 21 Feb 2023; Revised version received: 28 Dec 2023; Accepted: 28 Dec 2023
Published online: 28 December, 2023
![]()
ABSTRACT
Uterine rupture, a critical event during childbirth, poses significant challenges in familial and societal contexts. Despite concerted efforts to prevent such occurrences, inevitabilities arise, placing immense burdens on emergency healthcare teams, particularly in remote areas with inadequate facilities. What makes uterine rupture even more dangerous is the difficulty and the delay in diagnosis, especially in the unscarred uterus which invariably causes loss of the fetus in vivo and a high degree of maternal morbidity and mortality. This case series described three cases of rupture in the unscarred uterus, and their subsequent management and outcomes in a resource-constrained environment in Northeast India. Out of three cases, neonatal mortality was reported in all the cases, while maternal mortality was reported in one case. The findings underscore the critical need for heightened awareness, efficient diagnostic strategies, and improved healthcare infrastructure to address the complexities of uterine rupture in unscarred uteri, particularly in low-resource settings.
Keywords: unscarred uterus, rupture, emergency, mortality
INTRODUCTION
Rupture uterus is one of the most catastrophic events in obstetric practice putting the life of both the mother and the fetus in jeopardy and posing a great challenge to the health infrastructure and demanding great skills from the health care providers. Even in the most advanced countries, it is not completely avoidable and incidence is 2 per 100,000 women in the unscarred uteri.1 Various factors like malnutrition, delay in seeking care or delay in referral contribute to this disastrous outcome especially in rural areas, where the incidence is much higher and under reported. Here we present three cases of rupture in the unscarred uterus over a period of two years which presented to the district hospital in North Tripura, a hilly state in Northeast India.
LEARNING POINTS
1. Uterine rupture may occur even in unscarred uterus which may lead to fetal death in all cases.
2. Early surgical intervention of the rupture can save the mother’s life.
3. Early detection of the risk of an obstructed labour is a life saving measure for both fetus and mother.
CASE DESCRIPTION
Case 1
A 36-year-old multigravida G4P1L1A2 was referred from a primary health center due to prolonged labor and reduced fetal movements. The patient presented with a systolic blood pressure (SBP) of 100 mmHg, diastolic blood pressure (DBP) of 70 mmHg, heart rate of 120 beats/ minute, temperature of 99 degrees, respiratory rate of 20/minute. Abdominal examination revealed a tender, rigid abdomen with no ascertainable uterine contour. Fetal heart rate was absent, and fetal parts were not palpable due to abdominal guarding. Vaginal examination showed parous os with blood staining the examining finger, fetal head was high up in the pelvis, and cervical motion tenderness was positive. Based on the condition, laparotomy was performed which revealed approximately 3 litres of haemoperitonium with the dead fetus lying in the peritoneal cavity and a 10 cm anterolateral uterine rupture in the lower segment, placenta being attached to the fundus. Peripartum total hysterectomy was performed, 3 units of packed RBC and 2 units of fresh frozen plasma were transfused intraoperatively. The postoperative period and hospital stay was uneventful, and the patient was discharged on post-operative day 7.
Case 2
A G5P3L3 patient was admitted to the hospital after one day of labour pains, having been unsuccessful in delivering under the care of a traditional birth attendant. All her previous home deliveries were uneventful. Upon examination, her SBP was 90 and DBP was 60 mmHg, pulse rate 120 beats/minute, severe pallor, and generalized dehydration were evident. Abdominal examination revealed a distended abdomen with flanks full, lost uterine contour, and multiple fetal parts were palpable. Vaginal examination showed 5 cm cervical dilatation, 50 percent effacement, and a high fetal station. Immediate resuscitation with crystalloids was administered. Laparotomy showed a dead male fetus of 3.5 kg lying in the peritoneal cavity with umbilical cord and placenta attached along with 3 litres of haemoperitonium. Posterolateral rent was present in the uterus going up to the round ligament. Peripartum hysterectomy was performed, but postoperatively, the patient's vitals became unstable, and oxygen saturation dropped. Left sided broad ligament haematoma was noticed, so bilateral internal iliac artery ligation was done, but the procedure could not survive the patient.
Case 3
A G2A1 woman was referred from a primary health center due to 48 hours of vaginal leakage at 30 weeks of gestation. Initial examination indicated a SBP of 110 and DBP of 70 mmHg, heart rate of 90 bpm. Abdominal examination revealed fetus in the transverse lie with fetal heart rate of 110 beats per minute. Vaginal examination revealed a closed internal os with no active leaking. Ultra sonographic examination showed placenta in the fundal region and oligohydramnios with AFI of 3 cm. Patient was counseled regarding the poor fetal prognosis and was started on conservative treatment with antibiotics and fluids, neuroprotection with magnesium sulfate and corticosteroids two doses were also given. After 72 hours, repeat ultrasonography revealed no fetal heart rate and simultaneously patient started complaining of upper abdominal pain, not relieved with conservative treatment. Considering the transverse lie and prolonged leaking predisposing to chorioamnionitis, decision for laparotomy was taken. Intraoperatively, 2 litres of haemopertoneum was found with a rent in the fundus with a rent in the fundus of the uterus at the placental implantation site. A 1.7 kg dead fetus was delivered by lower segment caesarean section. The placenta invaded the uterine fundus, requiring partial removal for hemostasis. Post-fetal removal, uterine fundus and lower segment caesarean section incision repair were done. 3 units of packed red blood cells were transfused intraoperatively and post operative period was uneventful. Placental histopathology revealed abnormally adherent placentation, correlating to the check curettage performed before this present pregnancy thereby instigating the abnormal placentation.
DISCUSSION
Uterine rupture is the most feared complication in modern obstetrics and carries a grave prognosis, the possibility of such a complication is always to be borne in mind by the health care provider especially in a low resource setting so that it can be identified early and urgent referral can be done in a well equipped centre to deal with the problem.
Aggarwal et al. in their case series described a case of uterine rupture in multigravida with hydrocephalus, the diagnosis which got delayed due to atypical presentation.1 In our Case No. 1, the referral was delayed in case of multigravida with prolonged labour which in itself can be a predisposing factor to rupture uterus. However, immediate laparotomy and peripartum hysterectomy was instrumental in saving the life of the mother. Vernekar et al. in their case study on unscarred uterine rupture reported a maternal death rate of 30.8 %. In our Case No. 2, we encountered both maternal and neonatal mortality. In this case, delayed arrival in the hospital is the main reason for the poor outcome, other factors being poor nutritional and anaemic status, lack of knowledge and improper attitude towards the possible complications of child birth from a community perpsective.2 Trivedi et al. in their case series of unscarred uterine rupture in the primigravida describes three case in which successful repair could be done in two cases and peripartum hysterectomy was done in one case.3 Our Case No. 3 demonstrates that early decision for laparotomy is required even if fetus is not considered mature in a case of chorioamnionitis, as it is paramount to save the life of the mother.
Although presence of uterine scar is the prime factor in uterine rupture,4 our cases demonstrate that it is important to keep in mind the possibility of rupture in the unscarred uterus also, especially in a low resource setting where patient presents in a very advanced state of pathology.5 Prolonged rupture of membranes before term pregnancy not resulting in spontaneous labour should raise the suspicion of uterine rupture even in the unscarred uterus.6, 7
Conclusion
Rupture in an unscarred uterus is a complicated event and requires immediate diagnosis and surgical intervention to avert maternal morbidity and mortality, requiring the multidisciplinary support of all the health care providers including blood products and the different presentations of the cases are to be borne in mind to successfully overcome the unintended outcome.
Acknowledgments
I would like to thank the patients and the next of kin (in case of deceased patient) in preparing this case series.
Funding
No external funding was received for preparing this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Ethical Approval
Consent was obtained from the patients.
ORCID iD
Pushpal Chowdhury https://orcid.org/0000-0002-0377-2714
References
1. Vandenberghe G, Vierin A, Bloemenkamp K, Berlage S, Colmorn L, Deneux-Tharaux C, Donati S, Gissler M, Knight M, Langhoff-Roos J, Lindqvist PG, Maier B, van Roosmalen J, Zwart J, Roelens K; INOSS (the International Network of Obstetrics Survey Systems). Incidence and outcomes of uterine rupture in women with unscarred, preterm or prelabour uteri: data from the international network of obstetric survey systems. BJOG. 2023 Nov;130(12):1493-1501. DOI: https://doi.org/10.1111/1471-0528.17517.
2. Vernekar M, Rajib R. Unscarred Uterine Rupture: A Retrospective Analysis. J Obstet Gynaecol India. 2016 Oct;66(Suppl 1):51-4. DOI: https://doi.org/10.1007/s13224-015-0769-7.
3. Trivedi K, Anand S, Monalisa. Case series of unscarred uterine rupture in primigravida. J Family Med Prim Care. 2022 Jul;11(7):4079-4082. DOI: https://doi.org/10.4103/jfmpc.jfmpc_2325_21.
4. Mishra M, Mala YM. Idiopathic spontaneous rupture of unscarred uterus in a primigravida in active labour. Int J Surg Case Rep. 2022 Nov;100:107749. DOI: https://doi.org/10.1016/j.ijscr.2022.107749.
5. Takai IU, Abubakar A. Combined uterine and urinary bladder rupture: an unusual complication of obstructed labor in a primigravida. Int J Womens Health. 2016 Jul 21;8:295-8. DOI: https://doi.org/10.2147/IJWH.S104354.
6. Mourad WS, Bersano DJ, Greenspan PB, Harper DM. Spontaneous rupture of unscarred uterus in a primigravida with preterm prelabour rupture of membranes. BMJ Case Rep. 2015 Jun 8;2015:bcr2014207321. DOI: https://doi.org/10.1136/bcr-2014-207321.
7. Leroux M, Coatleven F, Faure M, Horovitz J. Rupture utérine bilatérale sur utérus gravide non cicatriciel en dehors du travail [Bilateral uterine rupture of an unscarred gravid uterus before labor]. Gynecol Obstet Fertil. 2014 Jun;42(6):454-7. French. DOI: https://doi.org/10.1016/j.gyobfe.2013.08.018.
|
|
|
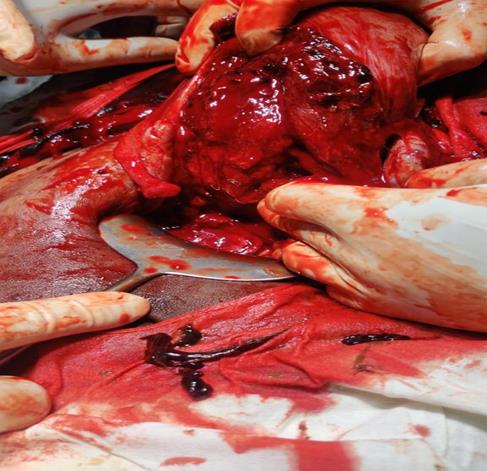
FIGURE 1 Intraoperative picture showing uterine rent |
|
|
|
FIGURE 2 Intraoperative picture showing rupture in the uterine fundus
|
(c) 2023 The Authors. Published by BSMMU Journal