Bangabandhu Sheikh Mujib Medical University Journal
Volume 16, Issue 4, December 2023
BRIEF ARTICLE
Association
of vitamin D level with systemic lupus erythematosus: A case-control study![]()
Mrinal Saha1![]() , Aparna Deb2
, Aparna Deb2![]() , Imtiaz Sultan2
, Imtiaz Sultan2![]() , Md. Abdur Razzaque3
, Md. Abdur Razzaque3![]() , Sakit Mahmud4
, Sakit Mahmud4![]() , Abu Kamran Rahul5,
Khaled Hassan6
, Abu Kamran Rahul5,
Khaled Hassan6![]() , Sujat Paul7
, Sujat Paul7![]()
1Department of Critical Care Medicine, Chittagong Medical College, Chattogram, Bangladesh
2Department of Medicine, Chittagong Medical College, Chattogram, Bangladesh
3Department of Rheumatology, Chittagong Medical College, Chattogram, Bangladesh
4Director General of Health Service, Dhaka, Bangladesh
5Department of Medicine, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
6Department of Endocrinology, Sheikh Hasina National Institute of Burn and Plastic Surgery, Dhaka, Bangladesh
7Marine City Medical College, Chattogram, Bangladesh
DOI: https://doi.org/10.3329/bsmmuj.v16i4.68428
Received: 26 Aug 2023; Revised version received: 17 Oct 2023; Accepted: 27 Nov 2023
Published online: 28 November, 2023
![]()
ABSTRACT
Background: Systemic lupus erythematosus (SLE) is a chronic autoimmune connective tissue disease. SLE patients are more prone to vitamin D deficiency because of their light sensitivity, renal involvement, and prolonged steroid use. This current study aimed to determine the relationship between vitamin D deficiency and SLE.
Methods: In this case-control study, 50 SLE patients (cases) and 50 healthy people (controls) were recruited. The reference value of vitamin D is as follows: normal ≥ 30 ng/ml, deficient ≤ 20 ng/ml, and insufficient 21-29 ng/ml.
Results: The mean (standard deviation) of vitamin D levels in SLE patients was 19.5 (5.3) ng/mL, which was significantly lower than those in healthy controls, 27.3 (10.0) ng/mL (P<0.001). The healthy controls had a higher proportion of people with normal vitamin D levels (≥ 30 ng/ml). We noticed a moderate negative correlation between vitamin D levels and fatigability, while a moderate positive correlation was seen with hemoglobin levels and the duration of sun exposure. However, in multiple logistic regression analysis all the associations mentioned above disappeared.
Conclusion: Although vitamin deficiency was found to be associated with SLE, its relationship disappears when the confounding by other variables is considered in the analysis.
Keywords: SLE, systemic lupus erythematosus, vitamin D deficiency
INTRODUCTION
Systemic lupus erythematous (SLE) is a common multisystemic autoimmune disease among Bangladeshi females. The relationship between vitamin D and SLE was first described in 1995 after discovering vitamin D receptors expressed by immune cells.1 As in other autoimmune diseases, vitamin D deficiency (VDD) could be one of the factors that may regulate SLE disease activity.2 Observation shows that VDD is more prevalent in Bangladesh, especially in females.3-6 VDD is common in SLE because of the avoidance of sun exposure owing to photosensitivity, use of sun protectors, second chronic renal insufficiency of lupus nephritis, and use of glucocorticoids and hydroxychloroquine medications that enhance the clearance of vitamin D.7
Researchers of previous studies have tried to establish the prevalence of VDD and its significance in various clinical aspects such as SLE disease activity, fatigability, and laboratory parameters.8, 9 A question that is yet to be answered is whether VDD indeed alters the course and prognosis of SLE. The answer to this query has a tremendous clinical impact on SLE treatment to potentiate therapeutic possibilities with vitamin D supplementation.10, 11
Regardless of whether VDD is a cause or consequence or both in SLE, its importance is almost undeniable. It is expected that vitamin D levels may differ among populations of different latitudes. Effects of vitamin D on SLE disease course represent an interesting area of research as it might allow a simple way to alleviate the disease course. The present study aims to determine the association of low vitamin D on disease activity among SLE patients attending a public medical college hospital
HIGHLIGHTS
1. The majority of SLE patients are vitamin D deficient.
2. Vitamin D levels are associated with fatigability and sun exposure duration.
METHODS
Study design
This case-control study was conducted in the departments of Medicine, Rheumatology, Nephrology, and Dermatology clinics of Chattogram Medical College Hospital, Bangladesh, from December 2017 to December 2018. One hundred patients were consecutively recruited, where 50 SLE patients were in the case group, and 50 were healthy individuals in the control group. Selected SLE patients fulfilled the revised American College of Rheumatology criteria for SLE classification and consented to participate in this study. Patients with end-stage renal disease, diabetes, severe sepsis, SLE with overlap, osteoporosis, osteomalacia, who were bed-ridden, and who received vitamin D within two months or having bisphosphonate, pregnant and lactating mothers were excluded from this study. Information were colleted on age, residence, education, economic status, and sun exposure time.
Data collection
Participants were interviewed using a semi-structured questionnaire. Diagnostic information, clinical and laboratory, were recorded. Four ml of venous blood was obtained from each participant in an 8-hour fasting state. Measurements of an inactive form of vitamin D3-25(OH)D levels in their sera were measured. The SLEDAI score was calculated based on patients' last 10-day clinical and lab parameters. The scoring system of SLE consisted of 105 points. The scores were categorized into (a) remission or no flare (scores 0-3), low (3-6), moderate (6-12), and high (>12) disease activity. Fatigue severity was assessed by a fatigue severity scoring system of seven questions (each question carried one point).
Data analysis
Data were analyzed using SPSS software, version 23. Continuous variables were expressed by mean and standard deviation (SD). Qualitative data were presented as numbers and percentages. Analysis was performed with the reference value of vitamin D: normal ≥ 30 ng/mL, insufficient 21-29 ng/mL, and deficient ≤ 20 ng/mL.12 Quantitative variables were compared using t test, and categorical data were compared using chi-square test. Pearson correlation was used to check the relationship between two continuous variables. Statistical significance was set at P < 0.05.
RESULTS
The mean (SD) age of cases and controls were 25.3 (9.8) and 29.3 (9.5) years. The mean (SD) of vitamin D levels were 19.6 (5.3) and 27.2 (10.0) among cases and controls, respectively (TABLE 1). This difference in mean levels was persistently observed in age groups, sexes, urban-rural residential areas, higher education, economic status, and one hour or more of sun exposure. However, all these significant differences disappeared when these were adjusted for confounding variables using a multiple logistic regression.
Sixty four percent of SLE patients and 36% of the controls had VDD. Thirty two percent of each group had insufficient vitamin D levels. Only 4% SLE patients had sufficient vitamin D levels, compared to 32% of controls (FIGURE 1). Vitamin D levels showed moderate positive correlations (r=0.47, P<0.01) with sun exposure time while negatively correlated with fatigue (r=-0.48, P<0.01) and erythrocyte sedimentation rate (r=-0.43, P<0.001) (TABLE 2).
An analysis among the cases showed a increading trend of vitamin D levels across four groups based on diseases severity: 16.6 ng/mL among severe SLE patients, 17.9 ng/mL in moderate, 24.4 ng/mL among low severity, and 26.2 ng/mL among patients with remission. Cases with lupus cerebritis (17.1 ng/mL) and lupus nephritis (17.5 ng/mL), photosensitivity (17.8 ng/mL) had lower levels of vitamin D.
DISCUSSION
This case-control study observed a difference in the vitamin D levels among SLE patients compared to the healthy controls. However, all the differences disappeared after adjustment for the potential confounding by the available variables. A similar observation was identified in an Indian case-control study.13 Similar findings were observed in Saudi Arabia, China, and Bahrain.6, 14 In an Egyptian study, researchers showed that their control group had optimal vitamin D levels (79.0 ng/mL), significantly higher than the SLE group (17.6 ng/mL).10 In an Australian cohort, Yap et al. showed approximately 40%-96% of SLE patients to be vitamin D deficient. Hence, low vitamin D is a common finding in patients with SLE.7 However, it is debatable whether VDD is a cause or consequence of SLE. It is very challenging to establish vitamin D as a cause of SLE; instead, it is wise to mark VDD as a risk factor for poor SLE disease outcomes.
Surprisingly, younger participants of both cases and controls had lower vitamin D levels than the older participants. This may be due to multiple factors that vary from person to person, e.g., season, sun exposure, and skin complexion. However, a large study from Lebanon found that older adults are more vitamin D deficient.15, 16
The lower vitamin D level in women might be attributed to their lifestyle, similar to the findings of another study on female garment workers.4 The people in rural areas are supposed to have more exposure to the sun. As a result, their vitamin D level should be higher than those living in urban areas. Surprisingly, we found a lower level of vitamin D among rural people. There are lines of evidence that adequate sun exposure improves vitamin D levels.17-18 In the current study, the individuals with less sun exposures had significantly lower vitamin D levels among both groups. But the differences did not persit when confounding by other variables were considered. Disease activity levels might be one of the major contributors to this.7, 8, 10 However, there are conflicting studies11, 14 that warrants resolution using well-designed studies.
Conclusion
Although this study’s representativeness is limited, we conclude that the SLE cases had lower levels of vitamin D. However, adjustment of the differences by potential confounders eliminated this difference. Given that studies around the world provided conflicting findings, a well-designed study ensuring representation of the cases and controls might provide a workable solution.
Acknowledgments
We thank Professor Dr. Asok Kumar Dutta for his kind supervision during the study. We also acknowledge Dr. Fazle Rabbi Chowdhury and Dr. Nazmul Hasan for reviewing the manuscript.
Author Contributions
Conception and design: MS, AD, IS, AR. Acquisition, analysis, and interpretation of data: MS, AD, IS, AR. Manuscript drafting and revising it critically: MS, AD, IS, AR, AKR, SM, KH, SP. Approval of the final version of the manuscript: MS, AD, IS, AR, AKR, SM, KH, SP. Guarantor of accuracy and integrity of the work: MS, AD, IS, AR, SP.
Funding
This study received no funding.
Conflicts of Interest
The authors declare no conflict of interest.
Ethical Approval
Before starting this study, the study protocol was reviewed and approved by the Research Technical Committee, Ethical Committee, and a Peer Review Committee of Chattogram Medical College (Ref no M/PG/2017/366 Date 27/12/2017). Informed verbal consent was taken from every patient. The purpose and procedures were briefly explained to all participants. The final database and report did not contain the names of the participants.
ORCID iDs
Dr. Mrinal Saha https://orcid.org/0000-0003-0682-9779
Dr. Aparna Deb https://orcid.org/0000-0002-4345-1843
Dr. Imtiaz Sultan https://orcid.org/0000-0003-4938-8125
Dr. Md. Abdur Razzaque https://orcid.org/0000-0002-2395-542x
Dr. Sakti Mahmud https://orcid.org/0009-0001-1325-9519
Dr. Khaled Hassan https://orcid.org/0000-0003-4838-0033
Dr. Sujat Paul https://orcid.org/0000-0002-2727-8489
References
1. Sakthiswary R, Raymond AA. The clinical significance of vitamin D in systemic lupus erythematosus: a systematic review. PLoS One. 2013;8(1):e55275. DOI: https://doi.org/10.1371/journal.pone.0055275.
2. Alexander T, Radbruch A, Hiepe F. Pathogenese des systemischen Lupus erythematodes [Pathogenesis of systemic lupus erythematosus]. Z Rheumatol. 2015 Apr;74(3):183-190. German. DOI: https://doi.org/10.1007/s00393-014-1456-2.
3. Islam QT, Amin MR. Vitamin D deficiency- current status and its impact in clinical medicine. Bangladesh Journal of Medicine. 2017;28(1):1-3. DOI: https://doi.org/10.3329/bjmed.v28i1.31895.
4. Mahmood S, Rahman M, Biswas SK, Saqueeb SN, Zaman S, Manirujjaman M, Perveen R, Ali N. Vitamin D and Parathyroid Hormone Status in Female Garment Workers: A Case-Control Study in Bangladesh. Biomed Res Int. 2017;2017:4105375. DOI: https://doi.org/10.1155/2017/4105375.
5. Ahasan HN, Das A. Vitamin D deficiency in South Asian populations: A serious emerging problem. Journal of Enam Medical College. 2013;3(2):63-66. DOI: https://doi.org/10.3329/jemc.v3i2.16125.
6. Attar SM, Siddiqui AM. Vitamin d deficiency in patients with systemic lupus erythematosus. Oman Med J. 2013 Jan;28(1):42-47. DOI: https://doi.org/10.5001/omj.2013.10.
7. Yap KS, Northcott M, Hoi AB, Morand EF, Nikpour M. Association of low vitamin D with high disease activity in an Australian systemic lupus erythematosus cohort. Lupus Sci Med. 2015 Apr 8;2(1):e000064. DOI: https://doi.org/10.1136/lupus-2014-000064.
8. Rifa i A, Kalim H, Kusworini K, Wahono CS. Effect of vitamin D supplementation on disease activity (SLEDAI) and fatigue in systemic lupus erythematosus patients with Hipovitamin D: An open clinical trial. Indonesian Journal of Rheumatology. 2018;8(2). DOI: https://doi.org/10.37275/ijr.v8i2.59.
9. Yap KS, Morand EF. Vitamin D and systemic lupus erythematosus: continued evolution. Int J Rheum Dis. 2015 Feb;18(2):242-249. DOI: https://doi.org/10.1111/1756-185X.12489.
10. Abaza NM, El-Mallah RM, Shaaban A, Mobasher SA, Al-Hassanein KF, Abdel Zaher AA, El-Kabarity RH. Vitamin D Deficiency in Egyptian Systemic Lupus Erythematosus Patients: How Prevalent and Does It Impact Disease Activity? Integr Med Insights. 2016 Sep 26;11:27-33. DOI: https://doi.org/10.4137/IMI.S40035.
11. Hamza RT, Awwad KS, Ali MK, Hamed AI. Reduced serum concentrations of 25-hydroxy vitamin D in Egyptian patients with systemic lupus erythematosus: relation to disease activity. Med Sci Monit. 2011 Dec;17(12):CR711-CR718. DOI: https://doi.org/10.12659/msm.882131.
12. Pludowski P, Takacs I, Boyanov M, Belaya Z, Diaconu CC, Mokhort T, Zherdova N, Rasa I, Payer J, Pilz S. Clinical Practice in the Prevention, Diagnosis and Treatment of Vitamin D Deficiency: A Central and Eastern European Expert Consensus Statement. Nutrients. 2022 Apr 2;14(7):1483. DOI: https://doi.org/10.3390/nu14071483.
13. Mandal M, Tripathy R, Panda AK, Pattanaik SS, Dakua S, Pradhan AK, Chakraborty S, Ravindran B, Das BK. Vitamin D levels in Indian systemic lupus erythematosus patients: association with disease activity index and interferon alpha. Arthritis Res Ther. 2014 Feb 10;16(1):R49. DOI: https://doi.org/10.1186/ar4479.
14. Farid E, Jaradat AA, Al-Segai O, Hassan AB. Prevalence of Vitamin D Deficiency in Adult Patients with Systemic Lupus Erythematosus in Kingdom of Bahrain. Egypt J Immunol. 2017 Jun;24(2):1-8. PMID: 29528574.
15. Khazaei Z, Khazaei S, Beigrezaei S, Nasri H. Vitamin D deficiency in healthy people and its relationship with gender and age. Journal of Parathyroid Disease. 2017;6(1):16-18. DOI: https://doi.org/10.15171/jpd.2018.06.
16. Arabi A, Baddoura R, El-Rassi R, El-Hajj Fuleihan G. Age but not gender modulates the relationship between PTH and vitamin D. Bone. 2010 Aug;47(2):408-412. DOI: https://doi.org/10.1016/j.bone.2010.05.002.
17. Karimzadeh H, Shirzadi M, Karimifar M. The effect of Vitamin D supplementation in disease activity of systemic lupus erythematosus patients with Vitamin D deficiency: A randomized clinical trial. J Res Med Sci. 2017 Jan 27;22:4. DOI: https://doi.org/10.4103/1735-1995.199089.
18. Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, Thomsen J, Charles P, Eriksen EF. Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited. J Intern Med. 2000 Feb;247(2):260-268. DOI: https://doi.org/10.1046/j.1365-2796.2000.00595.x.
|
TABLE 1 Vitamin D level (ng/ml) according to socio-demographic, clinical, and laboratory characteristics of the cases and controls |
|||
|
Variables |
Cases |
Controls |
P* |
|
(n=50) |
(n=50) |
||
|
Number (percent) |
|||
|
Age, years |
|
|
|
|
<25 |
30 (60.0) |
17 (34.0) |
0.01 |
|
25 or more |
20 (40.0) |
33 (66.0) |
|
|
Sex |
|
|
|
|
Male |
8 (16.0) |
10 (20.0) |
0.60 |
|
Female |
42 (84.0) |
40 (80.0) |
|
|
Residence |
|
|
|
|
Rural |
26 (52.0) |
18 (36.0) |
0.11 |
|
Urban |
24 (48.0) |
32 (64.0) |
|
|
Education |
|
|
|
|
Up to SSC |
42 (84.0) |
19 (38.0) |
<0.001 |
|
HSC and above |
8 (16.0) |
31 (62.0) |
|
|
Socio-economic |
|
|
|
|
Low/middle |
31 (62.0) |
17 (34.0) |
0.01 |
|
High |
19 (38.0) |
33 (66.0) |
|
|
Sun exposure |
|
|
|
|
<1 hour |
41 (82.0) |
18 (36.0) |
<0.001 |
|
≥1 hour |
9 (18.0) |
32 (64.0) |
|
|
Mean (standard deviation) of vitamin D level (ng/mL) |
|||
|
Overall |
19.6 (5.3) |
27.2 (10.0) |
<0.001 |
|
Age, years |
|
|
|
|
<25 |
20.2 (5.7) |
25.4 (9.0) |
0.04 |
|
25 or above |
18.6 (4.7) |
28.2 (10.5) |
<0.001 |
|
Sex |
|
|
|
|
Male |
20.2 (6.3) |
33.3 (8.5) |
0.002 |
|
Female |
19.4 (5.2) |
25.7 (9.8) |
0.001 |
|
Residence |
|
|
|
|
Rural |
18.8 (5.0) |
23.0 (7.6) |
0.05 |
|
Urban |
20.4 (5.7) |
29.7 (10.5) |
<0.001 |
|
Education |
|
|
|
|
Up to SSC |
19.7 (4.9) |
22.3 (7.1) |
0.10 |
|
HSC and above |
18.8 (7.5) |
30.3 (10.4) |
0.01 |
|
Socio-economic |
|
|
|
|
Low/middle |
19. 6 (5.6) |
24.5 (8.5) |
0.04 |
|
High |
19.5 (5.1) |
28.7 (10.5) |
<0.001 |
|
Sun exposure |
|
|
|
|
<1 hour |
19.3 (5.4) |
23.1 (9.4) |
0.29 |
|
≥1 hour |
21.0 (5.2) |
28.0 (10.0) |
0.046 |
|
*The Chi-square or t test, as appropria |
|||
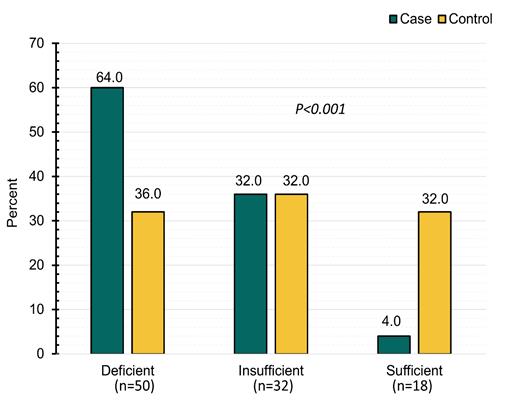
Figure 1 Vitamin D status among the case and controls (n=100)
|
Table 2 Correlation matrix between vitamin D levels and other variables (n=100) |
|||||||
|
Age |
Vitamin D |
Fatigue |
Hb |
ESR |
CRP |
Sun time |
|
|
1.0 |
0.26** |
-0.09 |
-0.05 |
-0.04 |
0.09 |
0.23* |
Age |
|
|
1.0 |
-0.48** |
0.31** |
-0.43** |
-0.12 |
0.47** |
Vitamin D |
|
|
|
1.0 |
-0.35** |
0.49** |
0.17 |
-0.56** |
Fatigue |
|
|
|
|
1.0 |
-0.54** |
-.21* |
0.36** |
Hb |
|
|
|
|
|
1.0 |
0.38** |
-0.61** |
ESR |
|
|
|
|
|
|
1.0 |
-0.29** |
CRP |
|
|
|
|
|
|
|
1.0 |
Sun time |
|
*P<0.05, **P<0.01 Hb indicates haemoglobin; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein. |
|||||||
(c) 2023 The Authors. Published by BSMMU Journal