|
Bangabandhu Sheikh Mujib Medical University Journal Volume 17, Issue 1, March 2024
BRIEF ARTICLE Infection
and co-infection patterns of common upper respiratory tract viruses in
patients with flu-like symptoms attending a fever clinic of a tertiary care
hospital during the COVID-19 pandemic
Md
Hossain Rahman
Department of Virology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
DOI: https://doi.org/10.3329/bsmmuj.v17i1.69132 Received: 27 Sep 2023; Revised version received: 13 Mar 2024; Accepted: 14 Mar 2024 Published online: 28 Mar 2024 Responsible
Editor: M Mostafa Zaman |
ABSTRACT
Background: More than 200 viruses can cause respiratory tract infections. It is clinically indistinguishable to differentiate SARS-CoV-2 viral infections from other viruses that cause flu-like symptoms. This study was done to determine the infection and co-infection patterns of common respiratory tract viruses in patients with flu-like symptoms attending a fever clinic during the COVID-19 pandemic.
Methods: A total of 288 participants attending the Fever Clinic of Bangabandhu Sheikh Mujib Medical University having respiratory symptoms were enrolled in this cross-sectional study done from November 2021 to March 2022. Nasopharyngeal swabs were obtained for molecular detection of selected respiratory viruses by multiplex polymerase chain reaction.
Results: The study participants were aged 18 to 72 (mean 33.2) years. SARS-CoV-2 infection was 16.7% among the participants, while other respiratory viruses were 24.3% that included rhinovirus (14.6%) followed by adenovirus (5.6%) and parainfluenza viruses (3.5%). SARS CoV-2 and rhinovirus (29.4%), adenovirus and rhinovirus (23.5%), and rhinovirus and parainfluenza virus (17.6%) were the most common co-infections among them (n = 17).
Conclusion: Nearly 17% infections were caused by SARS-CoV-2. Rhinovirus infection was the second most common of other upper respiratory viral infections. There is also evidence of co-infections between SARS-CoV-2 and other common upper respiratory tract viruses.
INTRODUCTION
The SARS-CoV-2 virus diverted focus from other widespread respiratory viral infections like respiratory syncytial virus (RSV) and influenza, clinically indistinguishable from COVID-19.1, 2 However, more than 200 viruses can cause respiratory tract infections.3 In developing countries, about 151 million/year children suffered from community-acquired pneumonia, most of which were due to respiratory viruses before the COVID-19 pandemic.4 Around 238 million people died in 2016 as a result of lower respiratory tract infections.5 Acute lower respiratory tract infections due to respiratory viruses accounted for about 60% of cases among children under five years from Bangladesh.6
The terms "flu-like symptoms" and "common cold" refer to groups of symptoms that are commonly known to be caused by viral infections of the upper respiratory tract. Rhinoviruses account for 30% to 70% of all respiratory infections, making them the most common cause of the common cold.3
Coronaviruses (except SARS-CoV-2) occur in 1 of 10 hospitalized children with respiratory tract infections and asymptomatic patients.7 The other common causes of respiratory sickness are influenza viruses A, human metapneumovirus (HMPV), adenoviruses, human parainfluenza virus (PIV) types,1-4 and RSV types A and B.3 Influenza and RSV are the pathogens most detected in respiratory viral infection in tropical countries.8
SARS-CoV-2 and influenza A co-infection were reported in China, Japan, Turkey, Iran, Spain, the USA, and Italy, where most patients needed ventilator support.11, 12, 13 However, the confection of the Influenza virus and SARS-CoV-2 was not found to be very common, and the disease severity was lower in Bangladesh.14 The interference of SARS-CoV-2 with other respiratory viral infections was thought to be due to the suppression of the circulation of influenza viruses, RSV and other acute respiratory viral pathogens during the pandemic coronavirus.15 Several studies showed worsening symptoms during co-infection2, 11, while others showed less disease severity.14, 16
A pre-pandemic study in Bangladesh showed that most detected viruses were rhinoviruses (22.0%), followed by RSV (8.9%), adenovirus (6.4%), PIV (6.1%), influenza virus (4.5%), and HMPV (4.5%).9 Monitoring of influenza like influcezalila illnesses reported 8% - 23% infections rates by influenza virus.10
More than three years have passed since the COVID-19 pandemic. Still, it is causing re-infection with the new variants in vaccinated people and those previously infected with SARS-CoV-2. Other respiratory viruses, such as human rhinovirus, adenovirus, parainfluenza virus, RSV, influenza A and B are causing infections. However, due to the severity of the pandemic, infection of other respiratory viruses remained unnoticed. The symptoms of other respiratory viruses are like COVID-19 infection. Hence, it is indistinguishable clinically. Co-infection of other respiratory viruses with SARS CoV-2 causes seven diseases.11, 17 In Bangladesh, limited studies have been done regarding coexistence of SARS-CoV-2 and other respiratory viruses. The present study was aimed to determine the infection and co-infection patterns of common respiratory tract viruses in patients with flu-like symptoms attending the Fever Clinic of a tertiary care hospital during the COVID-19 pandemic.
HIGHLIGHTS
1. Symptoms caused by common upper respiratory viruses and SARS-CoV-2 are clinically indistinguishable.
2. Multiplex PCR can differentiate them from the nasopharyngeal swabs.
3. Almost 17% had SARS-CoV-2 infections; commonest co-infections were “SARS-Cov-2+rhinoviruses” and “adenovirus + rhinoviruses”.
METHODS
This cross-sectional study was conducted among adult patients suffering from flu-like symptoms, such as chills or fever, cough, sore throat, runny or stuffy nose, headaches, body aches, fatigue, vomiting, and diarrhea, who attended the Fever Clinic of BSMMU from November 2021 to March 2022. Based on a previous study,6 the estimated sample size was 318. However, 288 participants could be enrolled.
Study samples were nasopharyngeal swabs for molecular detection of common respiratory viruses. All laboratory procedures were carried out at the Department of Virology, BSMMU, after obtaining ethical clearance.
Maintaining appropriate personal protective equipment (PPE) and the proper positioning of the patients, the sterile swab stick was inserted through the nostrils into the nasopharynx, and the swab was then rolled on the nasopharyngeal wall with enough pressure to remove cells from the mucosal surface in order to dislodge swab samples. Swab samples were kept in a single tube containing 1 ml of phosphate buffer saline (PBS), and the applicator stick was broken off. A cap tightly sealed sample tubes, and the samples were properly labelled. The specimens were kept in a box containing a frozen cold pack (at 4°C) and transported to the COVID-19 lab of the Department of Virology, maintaining the cold chain. After performing the SARS-CoV-2 multiplex PCR, the remaining samples were stored properly at -70°C freeze for further testing regarding other selected respiratory viruses.
The real-time multiplex PCR assay for SARS-CoV-2 was done by the QuantStudio 5 real-time PCR system (Thermo Fisher Scientific Inc., USA) using the Novel Coronavirus (2019-nCoV) nucleic acid diagnostic kit (PCR-Fluorescence Probing, Sansure Biotech Inc., China) following manufacturer instructions. For rhinovirus, adenovirus, RSV, Influenza A, Influenza B and parainfluenza virus, nucleic acid (DNA and RNA) was extracted from Nasopharyngeal samples using Quick-RNATM Viral Kit for detecting common upper respiratory tract viruses. The real-time multiplex PCR assay for influenza A virus, influenza B virus, respiratory syncytial virus, adenovirus, human rhinovirus, and mycoplasma pneumonia was performed by the Quantstudio 5 (Thermo Fisher Scintific Inc., USA) using the six RP (Respiratory Pathogens) nucleic acid diagnostic kit (PCR-Fluorescence Probing) (Sansure Biotech Inc., China) following manufacturer’s instructions. The real-time multiplex PCR assay for parainfluenza virus was performed by the Quantstudio 5 (Thermo Fisher Scientific Inc., USA) using the RealStar® PIV RT-PCR Kit 2.0 (Altona diagnostic GmbH, Germany) following manufacturer’s instructions.
Statistical analysis was done using the SPSS22 (IBM, USA) and Microsoft Excel. Number (%) were presented and compared using chi square or Fisher’s Exact test, as appropriate. A P value of <0.05 was considered significant.
RESULTS
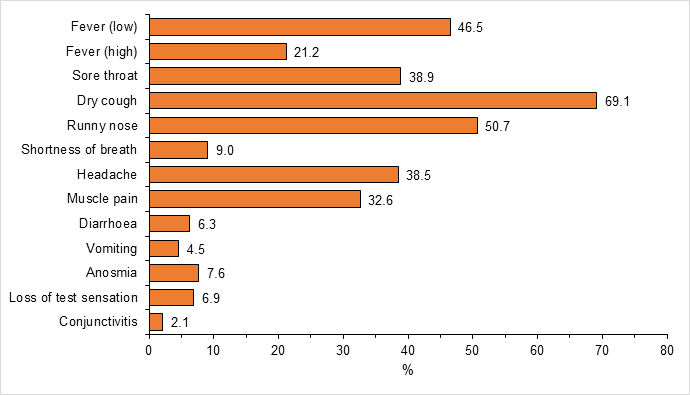
Out of the 288 participants aged 18 to 72 years, (mean 33.2, 178 (61.8%) were men. The mean duration of the flu-like symptoms was 4.7 days (range, 1 to 30 days). The most prevalent symptoms among study participants were dry cough 199 (69.1%) and runny nose 146 (50.7%) (Figure 1).
One hundred and eighteen (40.6%) had infections with common upper respiratory tract viruses (SARS-CoV-2, rhinovirus, adenovirus, RSV, parainfluenza virus and influenza B). Among the participants who had respiratory viral infections, 48 (16.7%) were positive for SARS-CoV-2 and 70 (24.3%) for other respiratory viral infections. The respiratory viral infection rates were similar in men and women (Table 1).
Seventeen patients had co-infections. The commonest types of co-infections were with SARS-CoV-2 and rhinovirus (29.4%), while the lowest prevalence of co-infection was with adenovirus and parainfluenza virus (5.7%) (Table 2).
DISCUSSION
It has been three years since the pandemic. During this pandemic, infection of other respiratory viruses remained unnoticed. This study was designed to determine common respiratory tract virus infection and co-infection patterns in patients with flu-like symptoms attending the Fever Clinic.
In this study, clinically, symptoms of SARS-CoV-2 and other respiratory viral infections were quite similar. Dry cough, low-grade fever, headache, and sore throat were the prominent symptoms of SARS-CoV-2 infection and other respiratory viral infections. These upper respiratory tract symptoms were consistent with previous studies.18, 19 Though anosmia is one of the most significant symptoms of COVID-19, it was found in very few patients in this study. However, symptoms may vary from variant to variant depending on geographical location, greater awareness, and more careful assessment of the patients.20 A study reported that anosmia can be a presenting symptom in other respiratory viral infections,21 and in this study, anosmia was also present in human rhinovirus, adenovirus & parainfluenza virus, which is like that study. Shortness of breath was a less presenting symptom in this study, as samples were collected from outpatient clinics; it is a more common symptom in hospitalized patients.
Because the study was done during the pandemic, SARS-CoV-2 infection was highest among the participants. In other respiratory viral infections, most infections occur with rhinovirus followed by adenovirus and parainfluenza viruses. Only one sample was found positive each for influenza B and RSV. Because RSV infection mostly occurs in children9 and influenza mostly occurs from May to September in Bangladesh,16 our study logically had a lower prevalence.
One previous study showed that women are more infected (13% to 26% higher) than men.22 which is not supported by our data probably because of the pandemicity. However, one Chinese study showed that men are more affected by SARS-CoV-2 infection than women. Therefore, these studies are not directly comparably.
SARS-CoV-2 co-infection with rhinovirus, adenovirus and parainfluenza virus was also found. Though in this study, only the pattern of infection was carried out, previous studies showed both mild and severe forms of diseases in cases of co-infection.11, 12, 13, 14, 16 In this study, no co-infection of SARS-CoV-2 was found with Influenza B and RSV as the infection rate of these viruses is low in this study. Though the co-infection of SARS-CoV-2 is associated with two or more respiratory viruses, no co-infection was associated with more than two viruses. This may be due to the smaller number of participants in this study.
Conclusion
Two in five Fever Clinic patients during the Covid-19 pandemic had common upper respiratory viral infections. Although, many viruses and bacteria that can cause upper respiratory infections could not be studied due to various constraints, our study reports co-existence of other common upper respiratory viruses like rhinovirus, adenovirus, and parainfluenza viruses with SARS-CoV-2. SARS-CoV-2 and rhinovirus and adenovirus co-infections were common among the participants. Future studies should cover wider range of microorganisms using longer sample size.
Acknowledgments
We are grateful to BSMMU for funding the research. We would also like to thank our teachers and colleagues of the Department of Virology, BSMMU and COVID laboratory, BSMMU for their kind co-operation.
Author contributions
Conception and design of the study: MHR, AN, MNI, SMRUI. Acquisition, analysis and interpretation of data: MHR, SS. Manuscript drafting and revising it critically: MHR, SS, AN, SMRUI, MNI. Approval of the final version of the manuscript: SS, AN. Guarantor of accuracy and integrity of the work: MHR, AN, SS, SMRUI, MNI.
Funding
This study was funded by BSMMU, Dhaka, Bangladesh as thesis grant for residents in 2023.study was funded by Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh as thesis grant for Residents in 2023.
Conflicts of interest
We do not have any conflict of interest.
Ethical approval
This study was reviewed and approved by the Institutional Review Board of BSMMU (Ref no. BSMMU/2021/12406, Date: 08/12/2021).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
References
1. Sarvepalli SS, Cruz AB, Chopra T, Salimnia H, Chandrasekar P. Striking absence of “usual suspects” during the winter of the coronavirus disease 2019 (COVID-19) pandemic 2020–2021. Infection Control & Hospital Epidemiology. 2021 Dec;42(12):1516-1517. DOI: https://doi.org/10.1017/ice.2021.303.
2. Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, Midgley CM, Kniss K, Burns E, Rowe T, Foust A, Jasso G. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic—United States, 2020–2021. Morbidity and Mortality Weekly Report. 2021 Jul 7;70(29):1013. DOI: https://doi.org/10.15585/mmwr.mm7029a1.
3. Rodgers L, Sheppard M, Smith A, Dietz S, Jayanthi P, Yuan Y, Bull L, Wotiz S, Schwarze T, Azondekon R, Hartnett K. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clinical Infectious Diseases. 2021 Jul 15;73(Supplement_1):S110-117. DOI: https://doi.org/10.1093/cid/ciab311.
4. Nascimento-Carvalho CM. Community-acquired pneumonia among children: the latest evidence for an updated management. Jornal de Pediatria. 2020 Apr 17;96:29-38. DOI: https://doi.org/10.1016/j.jped.2019.08.003.
5. Troeger C, Blacker B, Khalil IA, Rao PC, Cao J, Zimsen SR, Albertson SB, Deshpande A, Farag T, Abebe Z, Adetifa IM. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet infectious diseases. 2018 Nov 1;18(11):1191-1210. DOI: https://doi.org/10.1016/S1473-3099(18)30310-4.
6. Homaira N, Luby SP, Hossain K, Islam K, Ahmed M, Rahman M, Rahman Z, Paul RC, Bhuiyan MU, Brooks WA, Sohel BM. Respiratory viruses associated hospitalization among children aged< 5 years in Bangladesh: 2010-2014. PloS one. 2016 Feb 3;11(2):e0147982. DOI: https://doi.org/10.1371/journal.pone.0147982.
7. Heimdal I, Moe N, Krokstad S, Christensen A, Skanke LH, Nordbø SA, Døllner H. Human coronavirus in hospitalized children with respiratory tract infections: a 9-year population-based study from Norway. The Journal of infectious diseases. 2019 Apr 8;219(8):1198-1206. DOI: https://doi.org/10.1093/infdis/jiy646.
8. Caini S, de Mora D, Olmedo M, Portugal D, Becerra MA, Mejía M, Pacurucu MC, Ojeda J, Bonaccorsi G, Lorini C, Paget J. The epidemiology and severity of respiratory viral infections in a tropical country: Ecuador, 2009–2016. Journal of infection and public health. 2019 May 1;12(3):357-363. DOI: https://doi.org/10.1016/j.jiph.2018.12.003.
9. Chowdhury F, Shahid AS, Ghosh PK, Rahman M, Hassan MZ, Akhtar Z, Muneer SM, Shahrin L, Ahmed T, Chisti MJ. Viral etiology of pneumonia among severely malnourished under-five children in an urban hospital, Bangladesh. PloS one. 2020 Feb 4;15(2):e0228329. DOI: https://doi.org/10.1371/journal.pone.0228329.
10. Azziz-Baumgartner E, Alamgir AS, Rahman M, Homaira N, Sohel BM, Sharker MA, Zaman RU, Dee J, Gurley ES, Mamun AA, Fry AM. Incidence of influenza-like illness and severe acute respiratory infection during three influenza seasons in Bangladesh, 2008-2010. Bulletin of the World Health Organization. 2012;90:12-19. DOI: https://doi.org/10.2471/blt.11.090209.
11. Munivenkatappa A, Yadav PD, Swetha K, Jayaswamy M, Nyayanit DA, Sahay RR, Basavaraj TJ. SARS-CoV-2 & influenza A virus co-infection in an elderly patient with pneumonia. The Indian Journal of Medical Research. 2021 Jan;153(1-2):190. DOI: https://doi.org/10.4103/ijmr.ijmr_2711_20.
12. Zheng X, Wang H, Su Z, Li W, Yang D, Deng F, Chen J. Co-infection of SARS-CoV-2 and influenza virus in early stage of the COVID-19 epidemic in Wuhan, China. Journal of Infection. 2020 Aug 1;81(2):e128-129. DOI: https://doi.org/10.1016/j.jinf.2020.05.041.
13. Azekawa S, Namkoong H, Mitamura K, Kawaoka Y, Saito F. Co-infection with SARS-CoV-2 and influenza A virus. IDCases. 2020 Jan 1;20:e00775. DOI: https://doi.org/10.1016/j.idcr.2020.e00775.
14. Akhtar Z, Chowdhury F, Rahman M, Ghosh PK, Ahmmed MK, Islam MA, Mott JA, Davis W. Seasonal influenza during the COVID-19 pandemic in Bangladesh. PLoS One. 2021 Aug 3;16(8):e0255646. DOI: https://doi.org/10.1371/journal.pone.0255646.
15. Sominina AA, Danilenko DM, Stolyarov KA, Karpova LS, Bakaev MI, Levanyuk TP. Interference of sars-cov-2 with other respiratory viral infections agents during pandemic. EpidemiologiyaiVaktsinoprofilaktika. 2021;20(4):28-39. DOI: https://doi.org/10.31631/2073-3046-2021-20-4-28-39.
16. Cheng Y, Ma J, Wang H, Wang X, Hu Z, Li H, Zhang H, Liu X. Co‐infection of influenza A virus and SARS‐CoV‐2: A retrospective cohort study. Journal of Medical Virology. 2021 May;93(5):2947-2954. DOI: https://doi.org/10.1002/jmv.26817.
17. Dee K, Goldfarb DM, Haney J, Amat JA, Herder V, Stewart M, Szemiel AM, Baguelin M, Murcia PR. Human rhinovirus infection blocks severe acute respiratory syndrome coronavirus 2 replication within the respiratory epithelium: implications for COVID-19 epidemiology. The Journal of infectious diseases. 2021 Jul 1;224(1):31-38. DOI: https://doi.org/10.1093/infdis/jiab147.
18. Struyf T, Deeks JJ, Dinnes J, Takwoingi Y, Davenport C, Leeflang MM, Spijker R, Hooft L, Emperador D, Domen J, Tans A. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19. Cochrane Database of Systematic Reviews. 2022 1. (5). DOI: https://doi.org/10.1002/14651858.cd013665.pub3.
19. Sapra M, Kirubanandhan S, Kanta P, Ghosh A, Goyal K, Singh MP, Ratho RK. Respiratory viral infections other than SARS CoV-2 among the North Indian patients presenting with acute respiratory illness during the first COVID-19 wave. Virus Disease. 2022 Mar;33(1):57-64. DOI: https://doi.org/10.1007/s13337-022-00761-3.
20. Han AY, Mukdad L, Long JL, Lopez IA. Anosmia in COVID-19: mechanisms and significance. Chemical senses. 2020 Jul;45(6):423-428. DOI: https://doi.org/10.1093/chemse/bjaa040.
21. Agrupis KA, Villanueva AM, Sayo AR, Lazaro J, Han SM, Celis AC, Suzuki S, Uichanco AC, Sagurit J, Solante R, Yoshida LM. If Not COVID-19 What Is It? Analysis of COVID-19 versus Common Respiratory Viruses among Symptomatic Health Care Workers in a Tertiary Infectious Disease Referral Hospital in Manila, Philippines. Tropical Medicine and Infectious Disease. 2021 Mar 19;6(1):39. DOI: https://doi.org/10.3390/tropicalmed6010039.
22. Doerre A, Doblhammer G. The influence of gender on COVID-19 infections and mortality in Germany: Insights from age-and gender-specific modeling of contact rates, infections, and deaths in the early phase of the pandemic. Plos one. 2022 May 6;17(5):e0268119. DOI: https://doi.org/10.1371/journal.pone.0268119.
|
Figure 1The percentage of different symptoms of upper respiratory tract infections among study participants |
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||
(c) 2024 The Authors. Published by BSMMU Journal