Bangabandhu Sheikh Mujib Medical University Journal
Volume 16, Issue 4, December 2023
CASE REPORT
Right
hepatectomy with thrombectomy in treatment of hepatocellular carcinoma with
portal vein thrombosis: A case report![]()
Mohammad Saief Uddin![]() , Abdus Sakib
, Abdus Sakib![]()
Department of Hepatobiliary, Pancreatic and Liver Transplantation Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Correspondence to: Dr. Mohammad Saief Uddin, Email: drsaifuddin@bsmmu.edu.bd
DOI: https://doi.org/10.3329/bsmmuj.v16i4.70052
Received: 22 Nov 2023; Revised version received: 11 Dec 2023; Accepted: 18 Dec 2023
Published online: 20 December, 2023
![]()
ABSTRACT
Hepatocellular carcinoma (HCC) attacks the intrahepatic vasculature, particularly the portal vein. One of the most important criteria for a poor prognosis in individuals with HCC is the presence of portal vein tumour thrombus (PVTT). There is no global consensus or standard guidelines on the management of HCC with PVTT. We present a 48-year-old male manual labourer with a mass in the right hypochondriac region associated with dull, aching pain for four months. His preoperative preparation, involved addressing and rectifying any existing deficits. Standard precautions were taken for a major liver resection, specifically a right hepatectomy with the removal of a blood clot from the right portal vein. Postoperatively, the patient was mobilized on the first day, engaged in respiratory exercises, and received preventive measures against deep vein thrombosis. We have successfully performed a right hepatectomy with thrombectomy for HCC right lobe with PVTT, which showed a better outcome for the patient. He was leading a normal life at 14-day and 45-day follow-up visits.
Keywords: hepatocellular carcinoma, portal vein tumour thrombus, thrombectomy
INTRODUCTION
Hepatocellular carcinoma (HCC) is a widespread and serious healthcare problem globally. It is ranked as the sixth most diagnosed cancer. HCC is also the fourth leading cause of cancer-related deaths around the globe. 1 HCC often invades the intrahepatic vasculature, particularly the portal vein.1 Portal vein tumour thrombus (PVTT), on the other hand, is the most common type of macrovascular invasion, occurring in 44.0% to 62.2% among HCC patients, while hepatic vein tumour thrombus is rare, with an incidence of 1.4% to 4.9%, and inferior vena cava/intra-right atrial tumour thrombus is even rarer, with an incidence of 3% to 4%.2 PVTT is macroscopically classified into four types using medical imaging based on Chinese Cheng's classification.3 This classification includes four types (type I to IV) depending on the invasion of thrombus to surrounding vasculature, e,g. portal vein, and mesenteric vein. The presence of PVTT among HCC patients is a significant factor associated with poor prognosis.4
To our knowledge, there is no global consensus or existing standard guidelines for managing HCC with PVTT. To enhance the prognosis aggressive treatment options have been proposed in the Asia-Pacific region, including Bangladesh.5, 6 In addition to small-molecule targeted therapies like sorafenib and lenvatinib, clinical practices have gradually recognized treatments such as trans-arterial chemoembolization, radiotherapy, hepatic resection, and liver transplantation. Various studies are being carried out to improve the prognosis of HCC patients with PVTT with more aggressive treatment modalities like liver resection to transplantation. Thus, we have performed the right hepatectomy with thrombectomy for the HCC right lobe with PVTT (Type III that involved portal vein) for a better prognosis of such cases.
LEARNING POINTS
1. The presence of portal vein tumour thrombus is the most important criterion for poor prognosis of hepatocellular carcinoma.
2. The patient had satisfactory in-hospital outcomes after the right lobectomy with thrombectomy for the hepatocellular carcinoma right lobe with portal vein tumour thrombus.
3. The patient was leading a normal life at 14-day and 45-day follow-up visits.
CASE DESCRIPTION
A 48-year-old male, a manual labourer by profession, presented with a mass in the right hypochondriac region associated with dull aching pain for four months. Abdominal examination revealed a firm tender mass in the right hypochondriac region. On routine examination, haemoglobin was 10 g/dL, white blood cell count was 11,000; platelet count was 300,000 serum glutamic pyruvic transaminase was 200 U/L, and alpha-fetoprotein was 950.7 ng/mL. HBsAg was positive with undetected hepatitis B virus DNA. Abdominal ultrasound revealed an 83 mm × 56 mm mixed echogenic area in the right lobe of the liver.
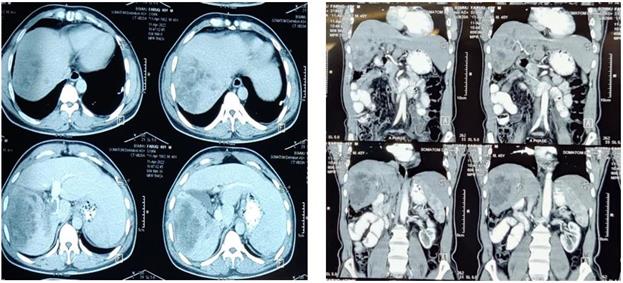
A computed tomography scan showed a space occupying lesion measuring about 7.8 cm × 5.5 cm × 8.0 cm involving segments V-VIII in the right lobe of the liver suggestive of HCC. In addition, a computed tomography scan showed a dilated portal vein containing a thrombus within the right branch and the main portal vein (type III). His Child-Turcotte-Pugh score was 6 and graded as class A (Child Pugh A).
CASE MANAGEMENT
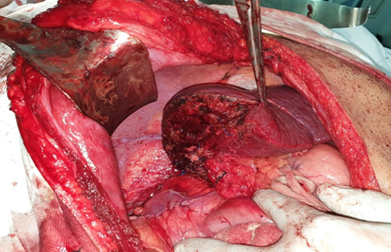
On laparotomy, a mass occupying almost the whole of the right lobe with compensatory hypertrophy of the left lobe of the liver was found. The patient underwent preoperative preparation, which involved addressing and rectifying any existing deficits. Standard precautions were taken for a significant liver resection, specifically a right hepatectomy with the removal of a blood clot from the right portal vein.
Cholecystectomy with right hepatectomy was done. On palpation of the portal vein at the junction of the division to the right portal vein, a thrombus was felt, which was extracted, and the right portal vein stump was closed with a 5/0 atraumatic proline. Portal clamping and length of operation were 14 and 150 minutes, respectively. Intraoperative blood loss was about 500 ml, and two units of blood were transfused per operatively.
The post-operative period was uneventful, and the patient was discharged on the seventh postoperative day. He was followed-up after 14 days and 45 days after the release from the hospital. There was no history of fever, vomiting, diarrhoea, constipation, or jaundice. On examination, abdomen was soft, not distended or tender. There was no sign of bleeding or discharge from the wound. The patient was encouraged to mobilize on the first day, engaged in respiratory exercises, and received preventive measures against deep vein thrombosis. The surgery of right hepatectomy with thrombectomy for HCC right lobe with PVTT (Type III) of the patient performed by us proved to be successful. On follow-up, the patient’s condition was improved. He was living a normal life.
DISCUSSION
Liver resection is the primary approach for managing HCC, offering the best potential for a cure.7 However, in western countries, the presence of PVTT has typically been considered a surgical contraindication according to the Barcelona Clinic Liver Cancer staging system.8 Consequently, most patients miss the opportunity for radical surgery, and the likelihood of a cure is exceedingly low. Nevertheless, advancements in surgical techniques and improvements in perioperative care have led to the adoption of more aggressive surgical resections for selected HCC patients with PVTT in specific medical centres. Surgical treatment becomes viable when the primary tumour and PVTT can be completely removed with no distant metastasis and liver function remains intact.9
Numerous studies, particularly in Asian liver centres, have assessed the effectiveness of surgical treatments for HCC. For instance, Kokudo et al. conducted a large retrospective study in Japan involving 6,474 HCC patients with PVTT. They compared outcomes of liver resection with alternative therapies.10 Their findings demonstrated that the surgical group, particularly those with good liver function (Child Pugh A), had a significantly longer mean survival time compared to the non-surgical group (2.9 years vs. 1.1 years). 10
In conclusion, liver resection with thrombectomy is a viable option when the tumour is operable because tumour thrombosis stemming from HCC typically does not deeply infiltrate the portal vein wall. This intensive treatment necessitates careful monitoring of the treatment's effectiveness to adjust the management plan for HCC with PVTT. The long-term benefits of this surgery need to be examined.
Acknowledgments
We would like to thank the patient and his attendant for their co-operation in preparing this case report.
Author Contributions
Conception and designed the experiments: MSU, AS. Performed the experiments: MSU. Manuscript writing and revising: MSU, AS. Approval of the final version: MSU, AS. Guarantor accuracy and integrity of the work: MSU, AS.
Funding
We did not receive any external funding for preparing this care report.
Conflicts of Interest
We declare no conflict of interest.
Ethical Approval
Consent was taken from the patent for preparing this case report. is a review work. Ethical approval was not necessary.
ORCID iDs
Danilo Mohammad Saief Uddin https://orcid.org/0009-0007-0023-6725
Abdus Sakib https://orcid.org/0009-0001-9633-5707
References
1. Global Burden of Disease Cancer Collaboration; Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabé E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castañeda-Orjuela C, Catalá-López F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, G/Hiwot TT, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Søreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017 Apr 1;3(4):524-548. DOI: https://doi.org/10.1001/jamaoncol.2016.5688.
2. Zhang ZM, Lai EC, Zhang C, Yu HW, Liu Z, Wan BJ, Liu LM, Tian ZH, Deng H, Sun QH, Chen XP. The strategies for treating primary hepatocellular carcinoma with portal vein tumor thrombus. Int J Surg. 2015 Aug;20:8-16. DOI: https://doi.org/10.1016/j.ijsu.2015.05.009.
3. Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, Wu MC, Cheng SQ. A new classification for hepatocellular carcinoma with portal vein tumor thrombus. J Hepatobiliary Pancreat Sci. 2011 Jan;18(1):74-80. DOI: https://doi.org/10.1007/s00534-010-0314-0.
4. Le Treut YP, Hardwigsen J, Ananian P, Saïsse J, Grégoire E, Richa H, Campan P. Resection of hepatocellular carcinoma with tumor thrombus in the major vasculature. A European case-control series. J Gastrointest Surg. 2006 Jun;10(6):855-862. DOI: https://doi.org/10.1016/j.gassur.2005.12.011.
5. Cheng S, Chen M, Cai J, Sun J, Guo R, Bi X, Lau WY, Wu M. Chinese Expert Consensus on Multidisciplinary Diagnosis and Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombus (2018 Edition). Liver Cancer. 2020 Jan;9(1):28-40. DOI: https://doi.org/10.1159/000503685.
6. Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, Tateishi R, Han KH, Chawla YK, Shiina S, Jafri W, Payawal DA, Ohki T, Ogasawara S, Chen PJ, Lesmana CRA, Lesmana LA, Gani RA, Obi S, Dokmeci AK, Sarin SK. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017 Jul;11(4):317-370. DOI: https://doi.org/10.1007/s12072-017-9799-9.
7. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011 Mar;53(3):1020-1022. DOI: https://doi.org/10.1002/hep.24199.
8. Forner A, Gilabert M, Bruix J, Raoul JL. Treatment of intermediate-stage hepatocellular carcinoma. Nat Rev Clin Oncol. 2014 Sep;11(9):525-535. DOI: https://doi.org/10.1038/nrclinonc.2014.122.
9. Cheng S, Chen M, Cai J; National Research Cooperative Group for Diagnosis and Treatment of Hepatocellular Carcinoma with Tumor Thrombus. Chinese expert consensus on multidisciplinary diagnosis and treatment of hepatocellular carcinoma with portal vein tumor thrombus: 2016 edition. Oncotarget. 2017 Jan 31;8(5):8867-8876. DOI: https://doi.org/10.18632/oncotarget.12817.
10. Kokudo T, Hasegawa K, Matsuyama Y, Takayama T, Izumi N, Kadoya M, Kudo M, Ku Y, Sakamoto M, Nakashima O, Kaneko S, Kokudo N; Liver Cancer Study Group of Japan. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 2016 Nov;65(5):938-943. DOI: https://doi.org/10.1016/j.jhep.2016.05.044.
|
|
|
|
A |
B |
|
FIGURE 1 Contrast CT scan of abdomen (A). axial view (B). coronal view showing SOL in the right lobe of the liver with a scattered area of necrosis within the lesion suggestive of hepatocellular carcinoma with dilated portal vein containing thrombus. |
|
|
|
|
|
A |
B |
|
FIGURE 2 (A) Shows abdomen opened with reverse L incision where tumour is occupying almost whole of the right lobe of liver, and (B) shows tumour thrombus extracted from portal vein. |
|
|
|
|
FIGURE 3 Picture showing after right hepatectomy with thrombectomy
|
(c) 2023 The Authors. Published by BSMMU Journal